Meet Dora Ogbonna, Ike Ogbonna, and Luann Zerefa, MS2s with the UCSF School of Medicine. We caught up with the team to see what they have been making in the Makers Lab.
Q: What did you create?
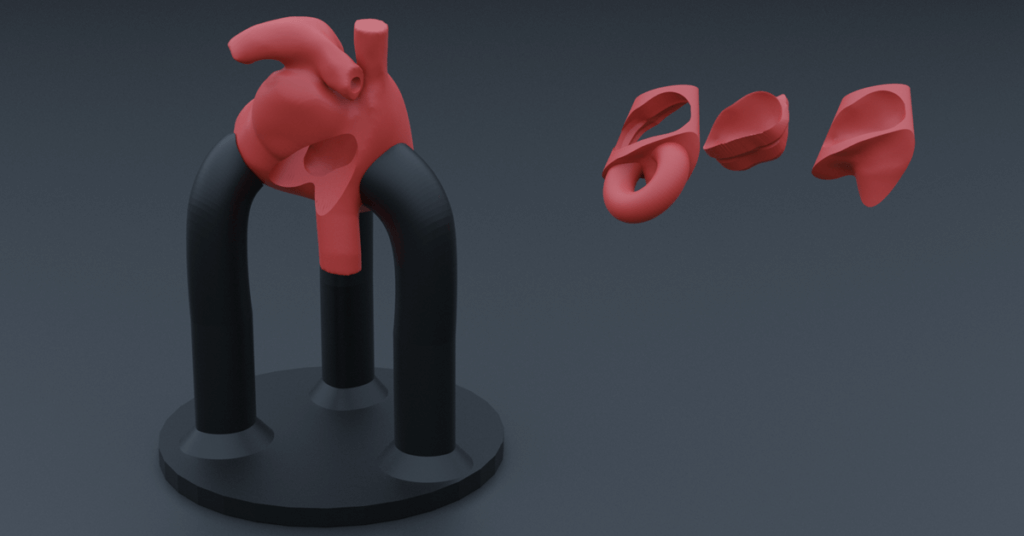
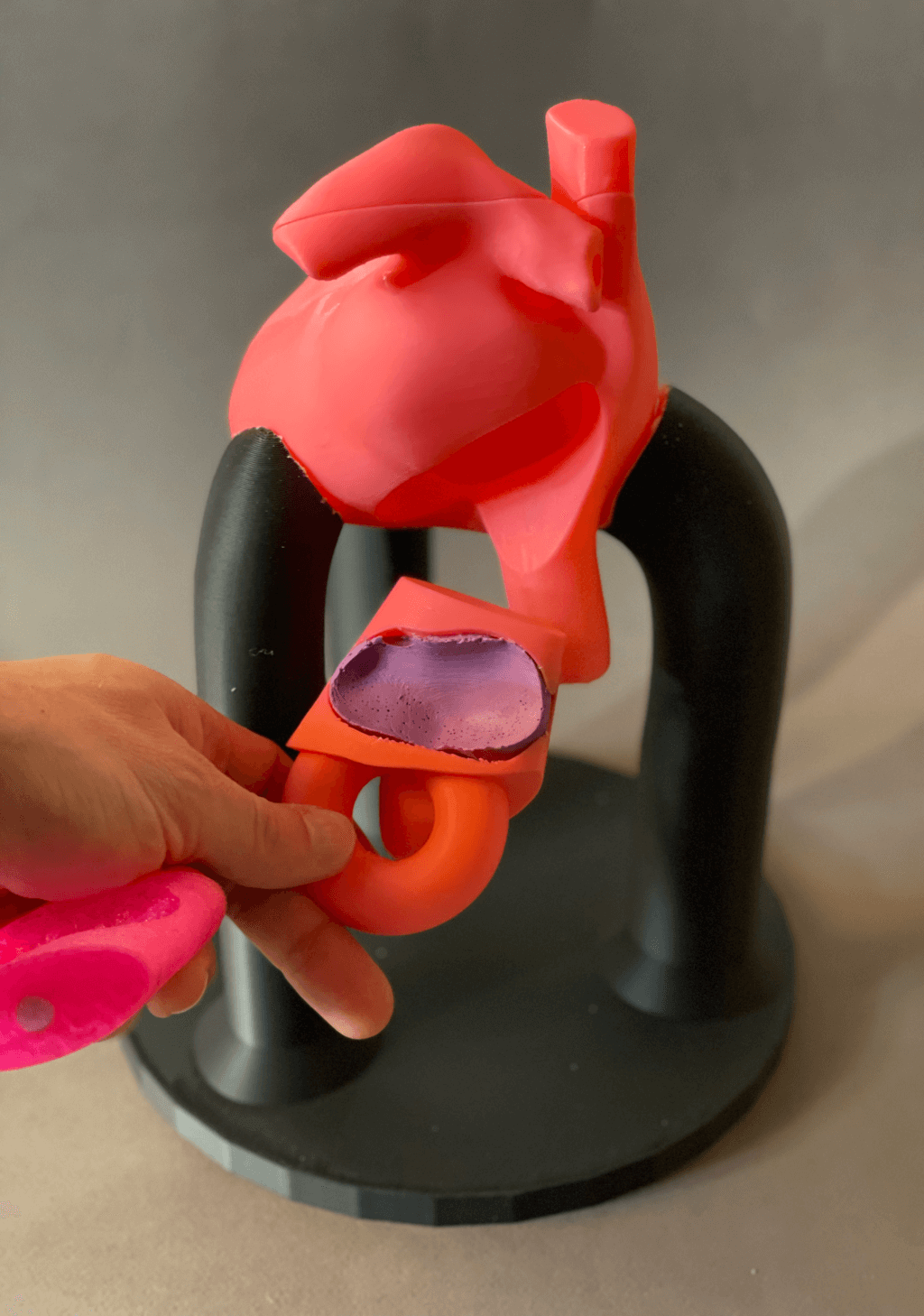
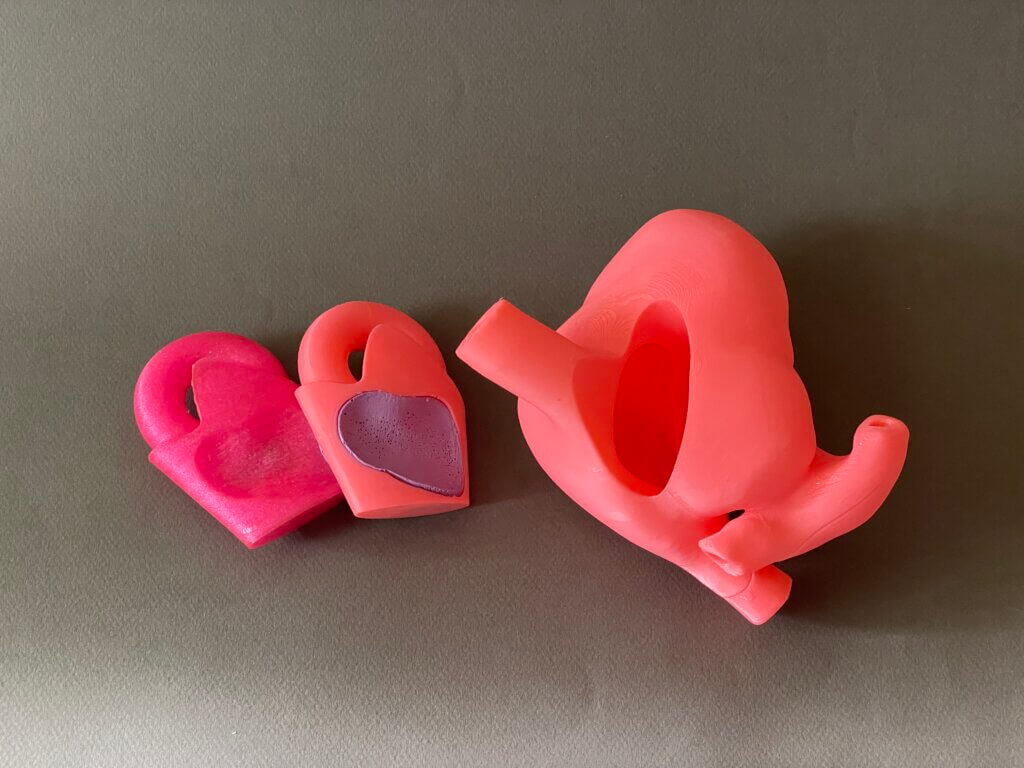
We partnered with Joshua Moss, MD, MS from the UCSF Division of Cardiology to create a to-scale model of the heart, focusing on the left atrium, so that fellows can practice catheter ablation techniques. Fellows can use our model to learn how to navigate their catheter while treating atrial fibrillation. This project was a result of the Advanced 3D Printing for Health Science Students elective.
Q: Why did you decide to create it?
We have learned about clinical cardiology and how closely tied it is to anatomical features in our coursework so far. We discussed the project with our faculty lead, Dr. Joshua Moss, a cardiac electrophysiologist, who described how electrophysiology fellows could benefit from hands-on learning using 3D printed models of the left atrium. After identifying this gap, together, we thought this could be a great project.
Q: What was your process like?
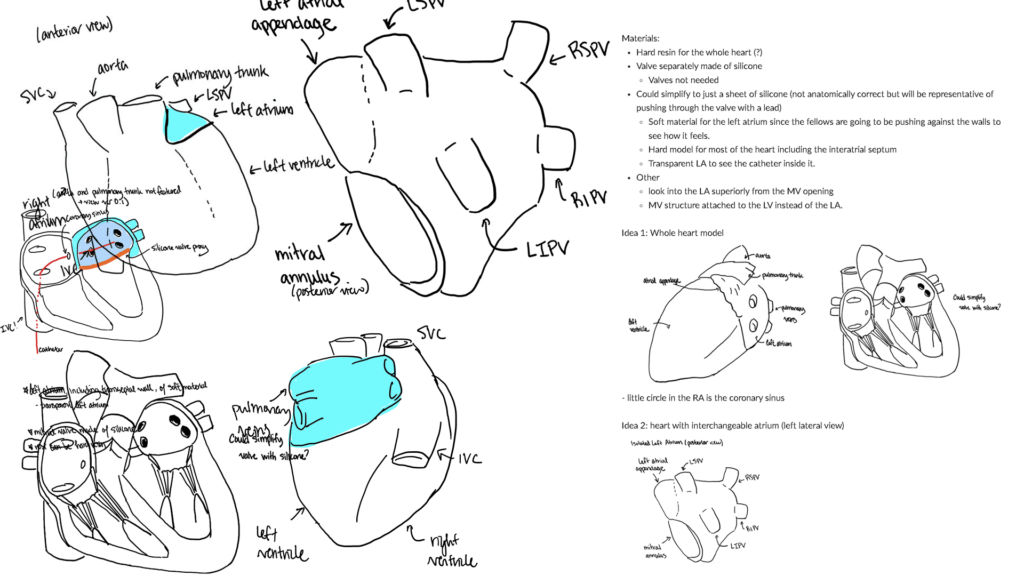
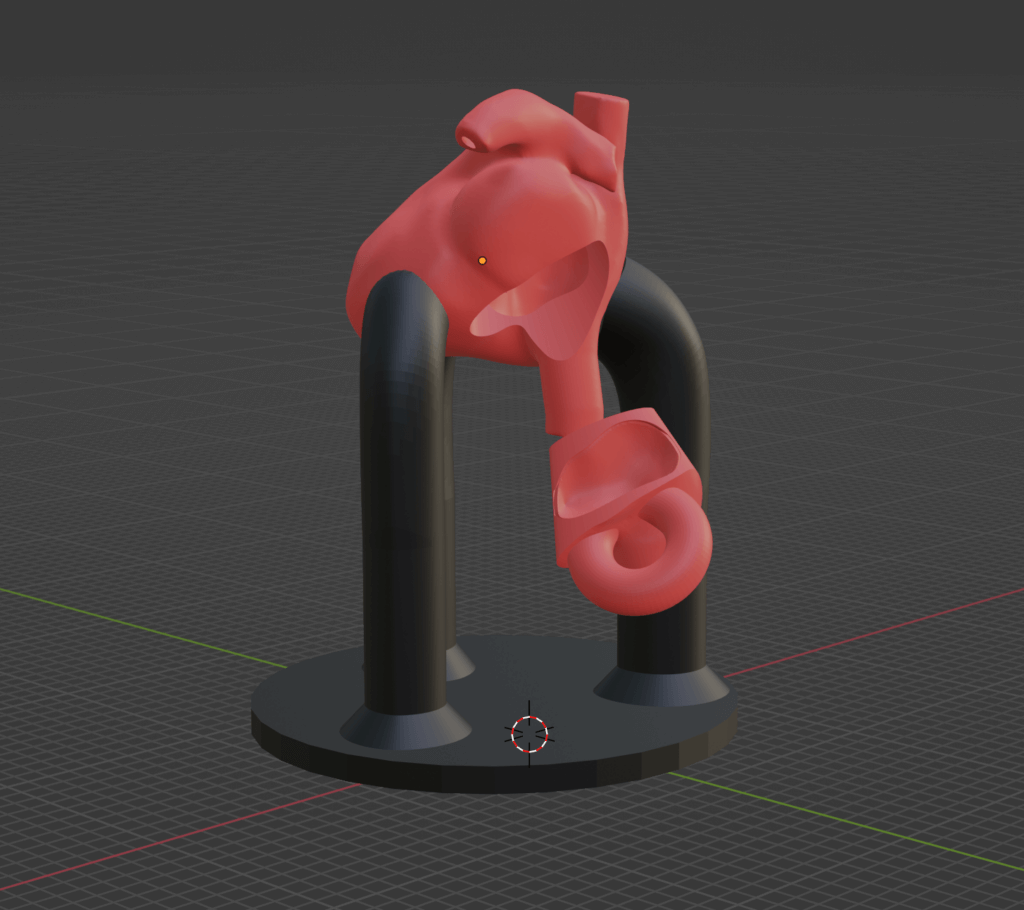
We began by doing a literature search where we looked at reports of similar projects of building full-scale and semi-flexible heart models. We wanted to gain information on challenges to this process, feedback from past similar projects, designs employed, characteristics of the design, and more. Using the information we attained from the literature search, we designed the model. First, we used an iterative approach involving planning, discussing, sketching designs, and noting challenges. We received feedback from the Makers Lab designer, Scott Drapeau, and our faculty lead, Dr. Joshua Moss to ensure we had an appropriate model design on paper. After that, we created a virtual model from patient MRI (Magnetic Resonance Imaging) data and our proposed design. We fine-tuned the design using 3D software, making sure that it had all the necessary anatomical features, and sent it in for 3D printing.
Q: What was the most challenging part of the process?
The most challenging part of the process was transferring the ideas we had from the sketched design to 3D format. We figured out quickly that this would take much more time and effort to create a successful model than we had initially planned. From there, we also found we had to troubleshoot to segment the heart from the MRI data using 3D Slicer software. However, we learned a lot about the process of design.
Q: What was your favorite part of the process?
Our favorite part of the process was getting to work together on this project and interacting with individuals who were specialists on various parts of the project. Dr. Moss provided insight into anatomical representation and clinical use. Scott Drapeau is phenomenal for his insights on best design choices, both for the 3D model and translating that to 3D printing. Thanks once again!
Q: How has this project contributed to your education?
This design has contributed to our education by allowing us to explore what is possible using 3D design. It can be a solution to a lot of problems that involves patient education, solidifying one’s skills in certain areas, and the like. In addition, we were also able to learn more about the heart and catheter ablation which was immensely helpful and insightful.

Q: What do you plan to create next?
We plan to continue updating the model we created with insight from fellows. We are still planning what our next big project is. With the skills we developed from this project, anything is possible in the future!
Acknowledgements
This project was made possible by a 2023 Innovations Funding for Education grant from the UCSF Academy of Medical Educators Innovations Funding Program.