This month’s maker is Ilana Roberts Krumm, MD, chief clinical fellow in the Division of Pulmonary, Critical Care, Allergy & Sleep Medicine with the UCSF Department of Medicine. Let’s take a look at what they made.
Q: What did you create?
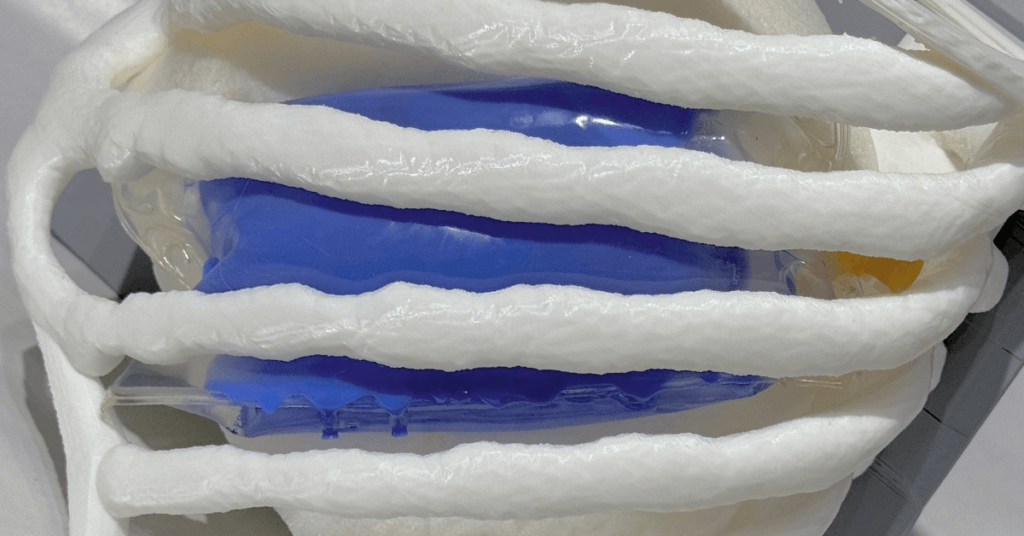
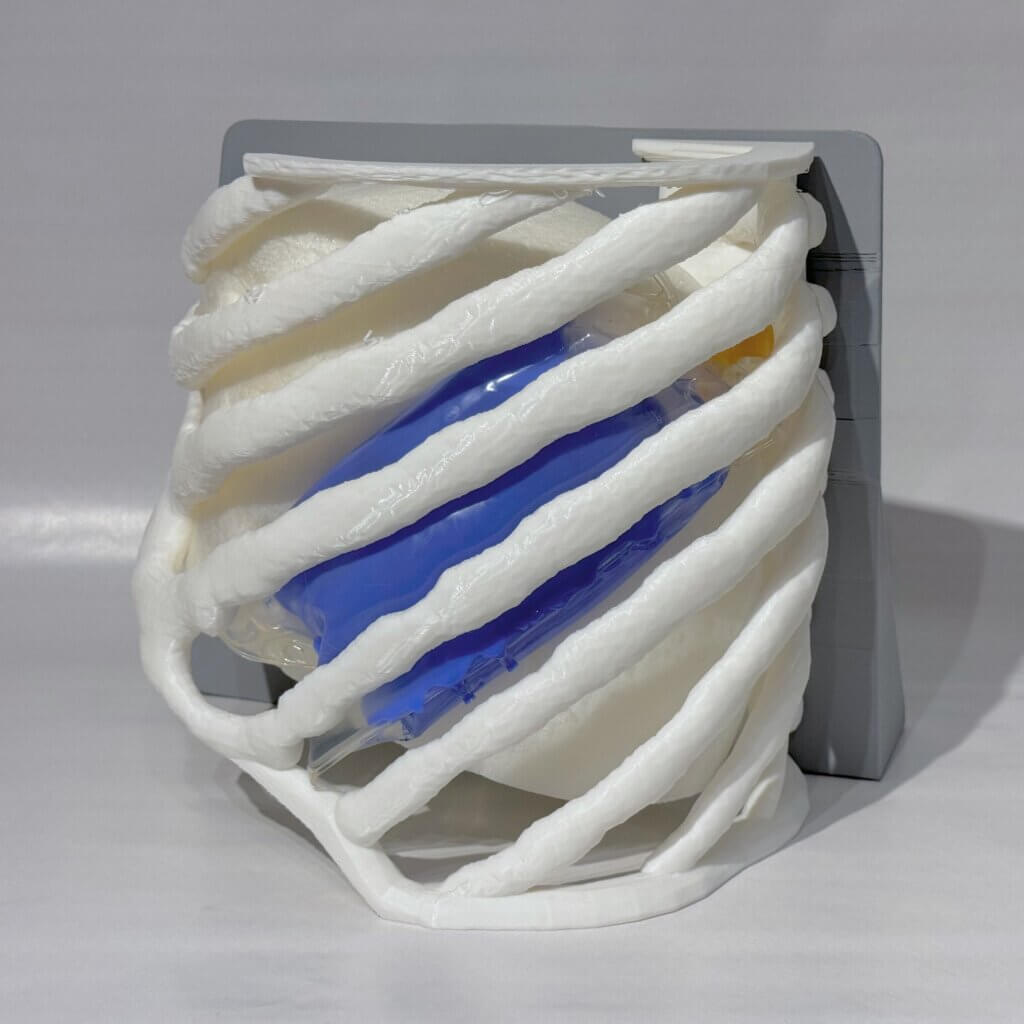
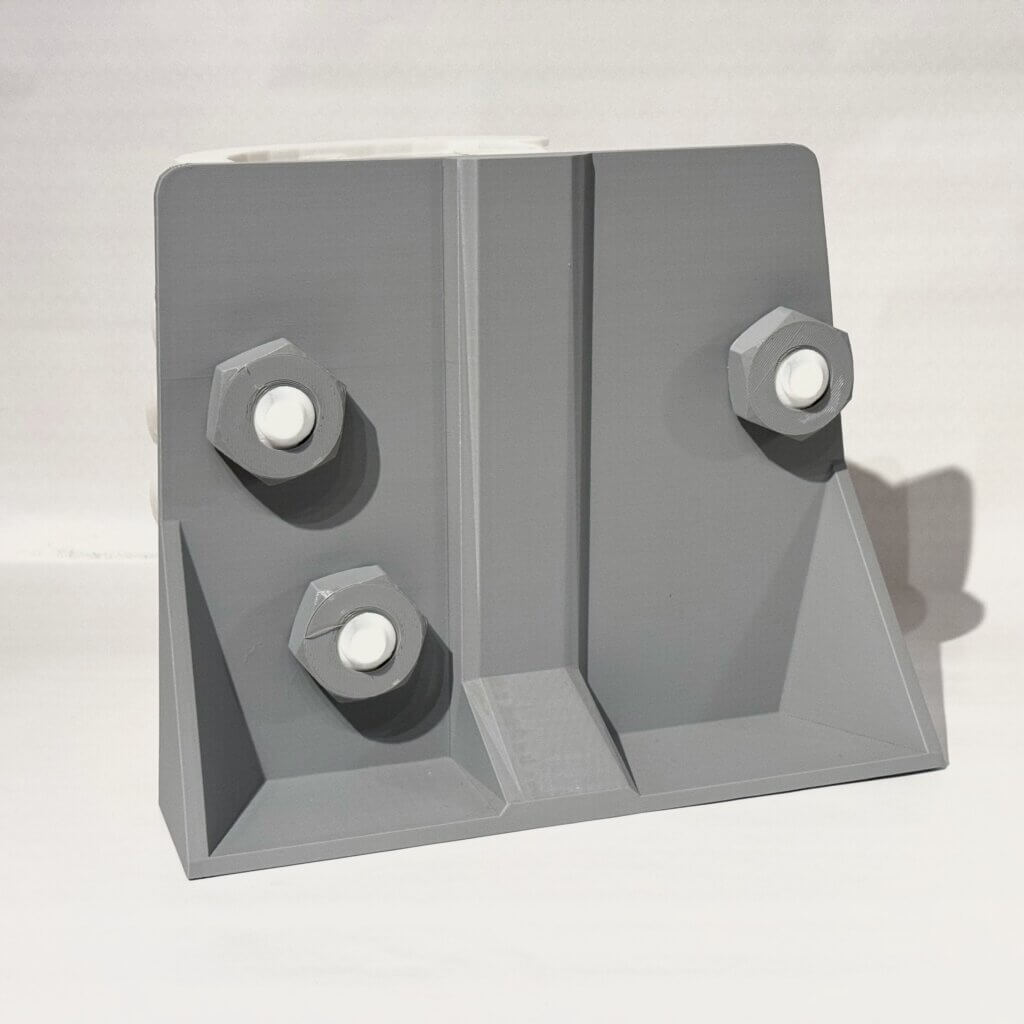
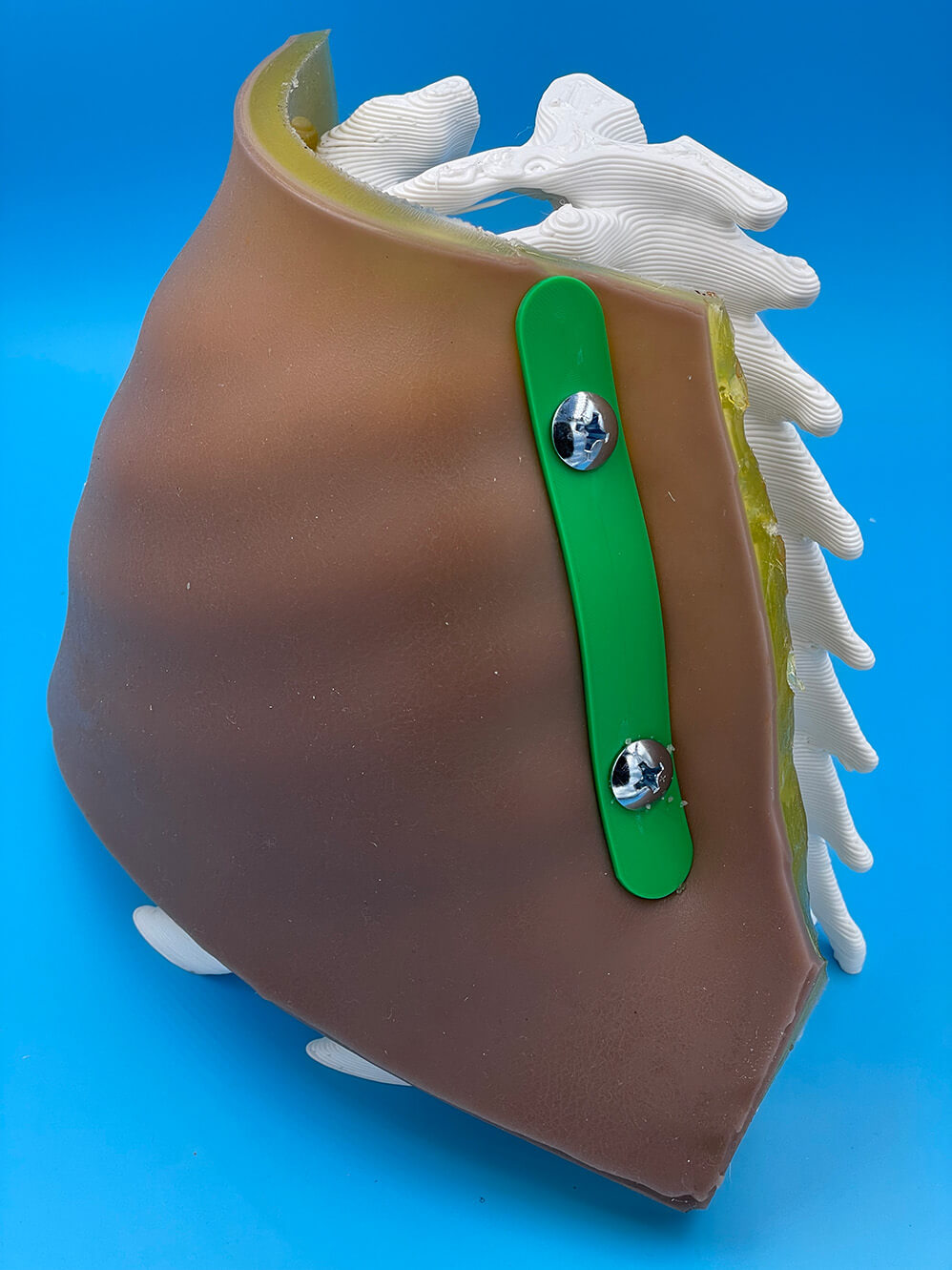
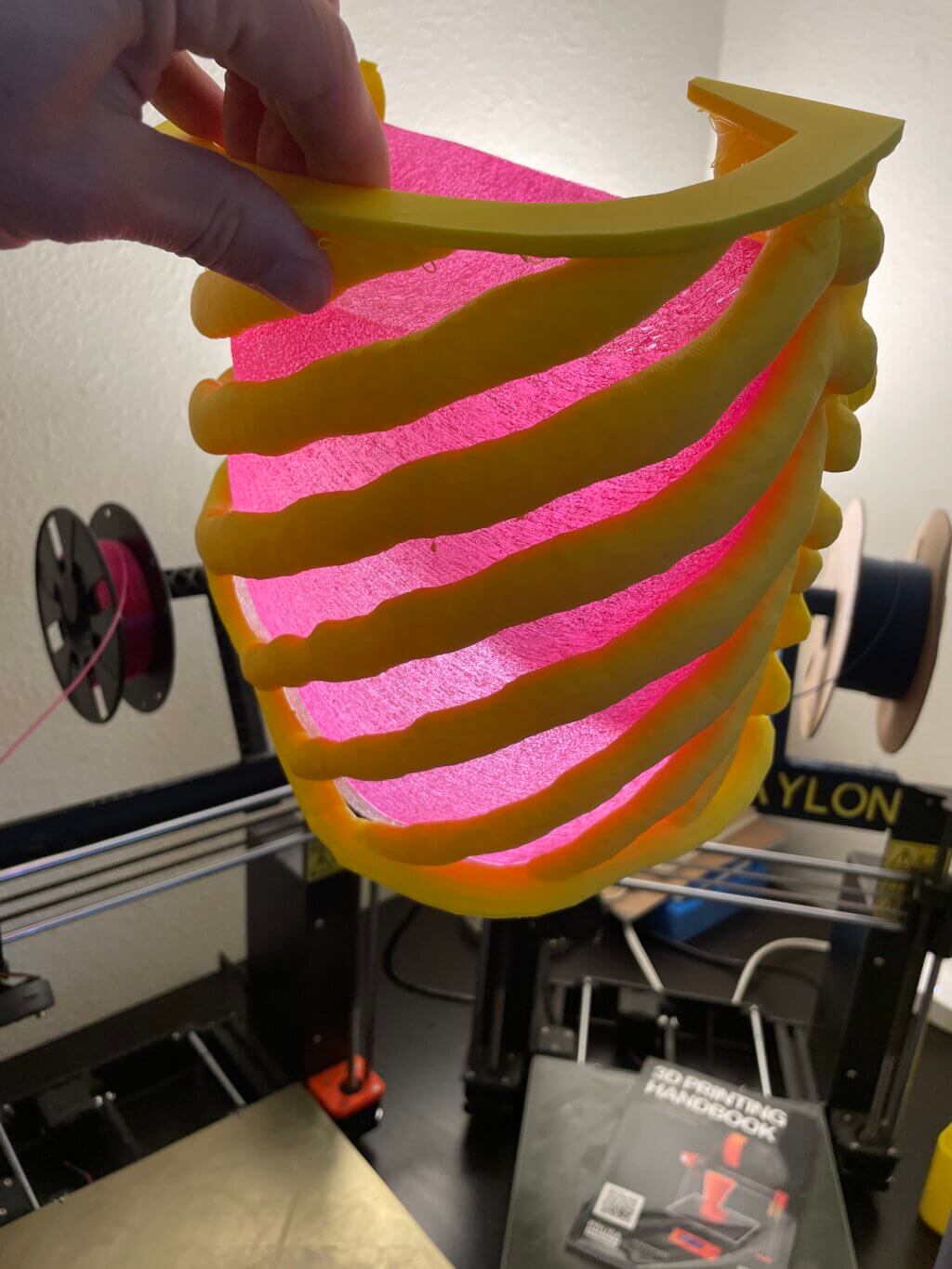
We created a pleural procedure simulator (affectionately dubbed “Explor-A-Thora”). This 3D-printed simulator offers realistic haptic feedback and ultrasound compatibility, providing a low-cost, high-fidelity alternative for medical training in pleural procedures.

Q: Why did you decide to create it?
We aimed to address the limitations of existing pleural procedure simulators, which cost thousands of dollars and lack realistic tactile feedback. Our goal was to create a more accessible and effective training tool that better mimics human tissue characteristics, while still being affordable for repeated use.
Q: What was your process like?
We collaborated closely with designer Scott Drapeau at the UCSF Makers Lab. Our process involved iterative prototyping, starting with initial designs that we co-created, and adjusting subsequent versions based on feedback we got from those who tested out our design.
Q: What was the most challenging part of the process?
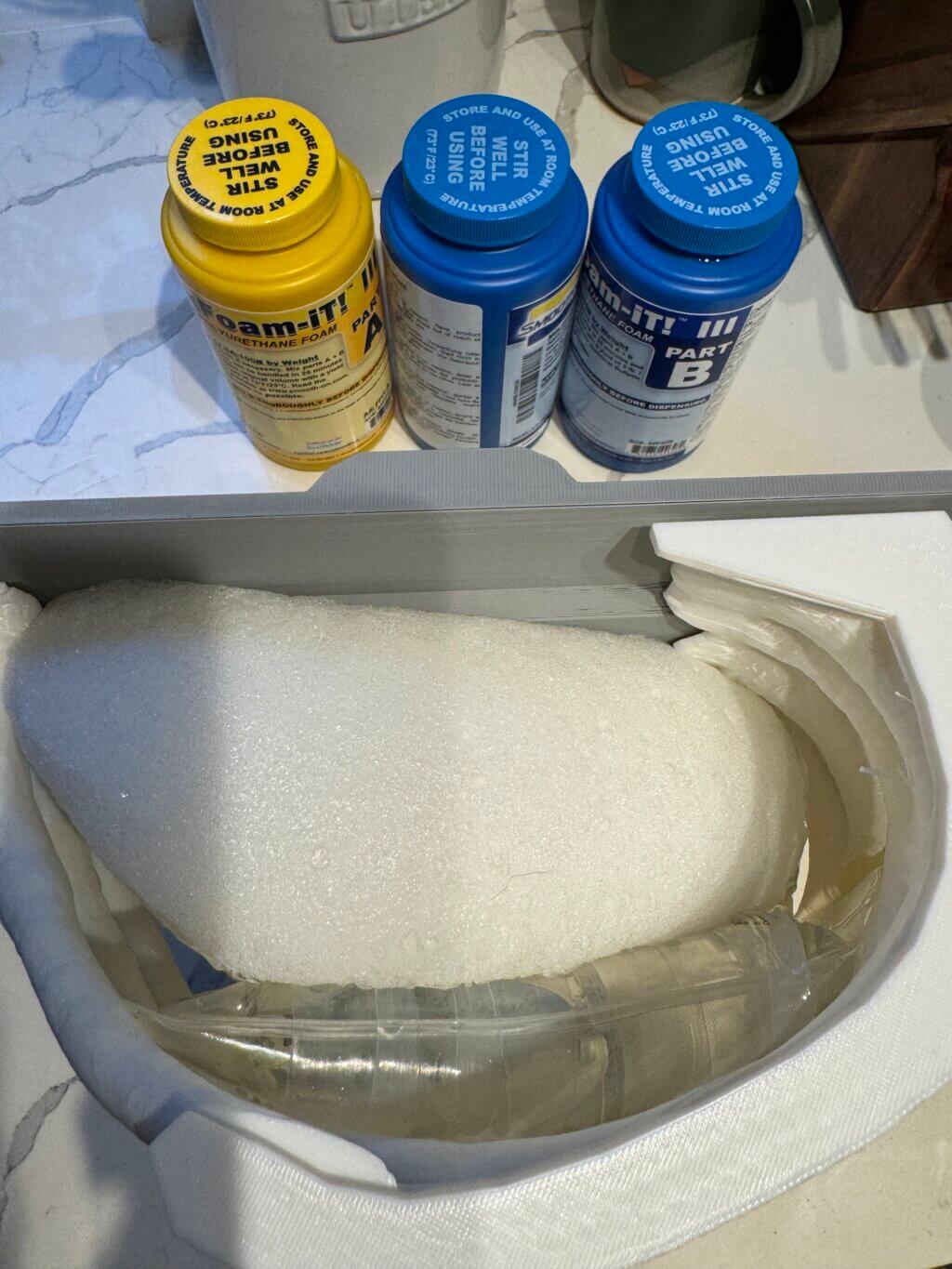
The most challenging part of the process was figuring out how to make the fluid pocket for our simulator. This took quite a bit of trial and error. Brainstorming with Scott, discussing possible materials and solutions, was integral to coming up with the ultimate design we used.
Q: What was your favorite part of the process?
The entire process was so much fun. It was satisfying seeing the tangible improvements in the simulator’s design after each iteration and hearing positive feedback from those who tested it. However the most gratifying part was seeing these models used for resident simulation sessions.
Q: How has this project contributed to your education?
For me personally this was an educational activity in the challenges of creating a simulator, particularly in the intricacies of designing tools that accurately mimic human physiological characteristics. This project has already been used for medical student and internal medicine resident education and has been deployed for several thoracentesis simulation sessions.
Q: What do you plan to create next?
Moving forward, I plan to develop more advanced versions of the simulator, incorporating features that allow for simulation of more complex pleural procedures like pleuroscopy. I also aim to create models that can simulate varying patient anatomies and complex pleural conditions such as adhesions and loculations.